By Akanimo Sampson
By utilising two types of stem cells, scientists from City University of Hong Kong (CityU) have developed a multi-pronged approach for concurrently rejuvenating both the muscle cells and vascular systems of the heart.
This came about as a medical emergency caused by severe cardiovascular disease, Myocardial Infarction (MI) can inflict permanent and life-threatening damage to the heart. The findings by a joint research team has given hope to develop a new treatment for repairing MI heart, as an alternative to the existing complex and risky heart transplant for seriously-ill patients.
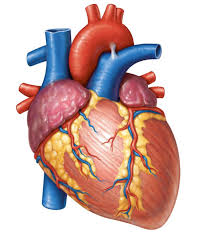
A Rael-Science post however says MI is a fatal disorder caused by a shortage of coronary blood supply to the myocardium. It leads to permanent loss of heart muscle cells (cardiomyocytes, CMs), and scar tissue formation, resulting in irreversible damage to cardiac function or even heart failure.
With limited therapeutic options for severe MI and advanced heart failure, a heart transplant is the last resort. But it is very risky, costly and subject to limited suitable donors. Therefore, stem cell-based therapy has emerged as a promising therapeutic option.
Dr. Ban Kiwon, a stem cell biologist from Department of Biomedical Sciences at CityU, has been focusing on developing novel stem cell-based treatments for cardiac regeneration. “Heart is an organ composed of cardiac muscles and blood vessels, where vessels are essential to supply oxygen and energy to the muscles. Since both cardiac muscles and vasculatures would be severely damaged following MI, the therapeutic strategies should focus on comprehensive repair of both at the same time. But so far the strategies only focus on either one”, he explains.
In this regard, Dr. Ban and his collaborators, including researchers from Konkuk University, The Catholic University of Korea, Pohang University of Science and Technology, and T&R Biofab in South Korea, have recently developed a multipronged approach.
It aimed to concurrently rejuvenate both the heart muscles and the vasculatures by utilising two major types of stem cells, namely human bone marrow derived mesenchymal stem cells (hMSCs) and cardiomyocytes derived from human induced pluripotent stem cells (hiPSC-CMs).
The hMSCs was employed in the study due to their prominent paracrine activity of secreting good proteins to promote the regeneration of blood vessels and the endothelial cell survival. And the hiPSC-CMs was utilised for their similarities with human primary CMs in terms of the expressions of cardiac-specific genes, structural proteins, ion channels, and more importantly, the spontaneous contraction.
While several previous studies described the beneficial effects of either hiPSC-CMs or hMSCs on MI separately, this is the first study to simultaneously examine the effects of these two distinct stem cells in cardiac repair.
The researchers have adopted a dual approach, in which the hMSCs and the hiPSC-CMs were delivered via two distinct routes. The hiPSC-CMs were intramyocardially injected directly into border zone of the rat’s heart, while the hMSCs-loaded patch was implanted on top of the infarct area, like a bandage.
The results showed that this dual approach led to a significant improvement of cardiac function and enhancement of vessel formation on a MI heart. The implanted hMSC-loaded patch not only provided a micro-environment which enhanced vascular regeneration as expected, but also improved the retention of hiPSC-CMs, ultimately augmenting heart function and restoring the injured myocardium.
Moreover, histological analyses results demonstrated that the implantation of hMSC-loaded patch has promoted the functional maturation of injected hiPSC-CMs. They became more elongated and rectangular in cell shape, appeared to be more organised in order, which were typical morphological characteristics of matured adult CMs.
Functional maturation of intramyocardially injected hiPSC-CMs is particularly important. It is because it can reduce potential risk of arrhythmias, meaning irregular heart contraction, which is a major cause of sudden cardiac death.
“We believe this novel dual approach can potentially provide translational and clinical benefit to the field of cardiac regeneration,” said Dr. Ban. “Based on the same principle, the protocol may also be utilised for repairing other organs including brain, liver and pancreas in which multiple types of stem cells are co-existing.”
The team is working on follow-up studies in larger animal model such as pigs. The patent application has been submitted.
Rael-Science however, pointed out that the research findings were published in scientific journal Nature Communications, titled Dual stem cell therapy synergistically improves cardiac function and vascular regeneration following myocardial infarction. Dr. Ban, together with Dr. Moon Sung-Hwan from Konkuk University School of Medicine and Professor Park Hun-Jun from The Catholic University of Korea, are the corresponding authors of the paper. The first authors are Park Soon-Jung from Konkuk University School of Medicine, Kim Ri Youn and Ph.D. student Lee Sunghun from CityU and Park Bong-Woo from The Catholic University of Korea.